Stroke epidemiology and prevention
Stroke is a devastating yet highly preventable disease. There are about 9,000 strokes every year in New Zealand, 30% of which are fatal in the first year and a further 70% of survivors are left with some level of disability. We are developing interventions that are potentially widely applicable, affordable, and cost-effective, even in low resource countries with no or little access to medical services.
Current projects
The Global Burden of Disease (GBD) stroke study aims to generate comparable information on disease burden in 21 regions of the world.
The GBD stroke study conducts systemic reviews of studies to estimate incidence, prevalence, case fatality and cause specific mortality for stroke risk factors. NISAN is the international headquarters for the stroke project and contributes to the GBD study. The project aims to collate the most comprehensive database of all epidemiological data on stroke. We invite researchers to submit relevant data on stroke incidence, prevalence and outcome.
Members of the stroke expert panel
The panel comprises approximately 300 experts around the globe.
Contact: Rita Krishnamurthi

Stroke and TIA are associated with a major economic burden, including emergency service use, hospitalisations, residential care, and other associated costs. Understanding the costs strokes and TIAs impose on the healthcare system and the people of New Zealand is critical for helping to identify and implement cost effective strategies that can reduce this burden.
The ARCOS V Programme is structured around four interlinked studies addressing the following aims: (Study 1) determining population-based estimates of stroke and TIA mortality and functional outcomes at 12 months and analysing 40-year trends in stroke burden, including healthcare use, and economic impact in the Auckland Region; (Study 2) determining the impact of pre-hospital pathways of stroke/TIA on their outcomes over the last 10 years (2011-2021); (Study 3) estimating the national burden of acute stroke, and (Study 4) determining the effectiveness of health and wellness coaching (HWC) in improving lifestyle behaviour to reduce the risk of stroke after a minor stroke or TIA.
Programme coordinator
Rita Krishnamurthi, AUT
Programme manager
Bala Nair, AUT
Principal investigators
- Professor Valery Feigin, AUT
- Associate Professor Rita Krishnamurthi, AUT
Project collaborators
- Professor Suzanne Barker-Collo, University of Auckland
- Dr Braden Te Ao, University of Auckland
- Professor Peter Barber, University of Auckland
- Professor Bruce Arroll, University of Auckland
- Associate Professor Daniel Exeter, University of Auckland
- Dr Yogini Ratnasabapathy, Waitemata District health Board
- Professor Jeroen Douwes, Massey University
- Associate Professor Annemarei Ranta, Otago University
- Dr Hinemoa Elder,
- Associate Professor Andrew Swain, AUT
- Dr Bronwyn Tunnage, AUT
- Associate Professor El-Shadan Tautolo, AUT
- Professor Craig Anderson, The George Institute
- Professor Amanda Thrift, Monash University
- Dr Derrick Bennett, Oxford University
- Professor Dominique Cadilhac, Monash University
- Professor Paul Brown, University of California, Merced
Timeline: March 2021 - February 2026
Funded by: Health Research Council of New Zealand
Budget: $4.9million
Study 2: Mapping the pre-hospital pathway of stroke
Contact: Dr. Bronwyn Tunnage
Principal Investigators: Prof. Valery Feigin (AUT); Dr. Bronwyn Tunnage (AUT); Assoc. Prof. Andrew Swain (Wellington Free Ambulance)
Aim/Summary: To determine the impact of pre-hospital pathways of stroke/TIA on their outcomes over the last 10 years (2011-2021). This study will determine how patients with stroke and TIA accessed the healthcare system, and the impact of the quality of their healthcare on the access to time-critical treatments in hospital. Cases for the study will be from the ARCOS V cohort. The five main objectives are to: (1) identify the referral pathway from the community; (2) establish the sensitivity and specificity of stroke/TIA recognition by paramedics; (3) evaluate the efficacy of the a New Zealand -developed paramedic acute assessment tool (PASTA) in identifying stroke-related large vessel occlusions; (4) determine the time to thrombolysis and endovascular clot retrieval associated with a paramedic-initiated bypass protocol policy; and (5) quantify the association between paramedic pre-arrival notification and in-hospital processes, treatment and outcome. These findings will inform EMS practice guidelines to improve outcomes of stroke/TIA.
Study 3: Determining national and regional (for all NZ DHBs) stroke incidence and mortality, and their determinants
Contact: Professor Jeroen Douwes (Massey)
Principal Investigators: Prof. Jeroen Douwes (Massey), Assoc. Prof. Anna Ranta (Otago University Wellington)
Aim/summary: This study will use robust and in-depth population-based data from ARCOS V and routinely collected national health and social data held in NZ’s IDI to determine national stroke incidence and mortality, and the impact of socio-economic status (SES) on stroke (with data for all DHBs).
Study 4: Trial of an Individualised Intervention for the Prevention of Stroke (TIIPS)
Contact: Dr. Devaki De Silva
Principal Investigators: Assoc. Prof. Rita Krishnamurthi (AUT); Prof. Suzanne Barker-Collo (Auckland); Prof. Valery Feigin (AUT)
Study manager: Dr Devaki De Silva / Jesse Dyer
Aim/Summary: To determine the effectiveness of health and wellness coaching (HWC) in improving lifestyle behaviour to reduce the risk of stroke after a minor stroke or TIA. This is a phase III, prospective, single blind, 2-arm randomised controlled trial to test the effectiveness of HWC for secondary prevention of stroke following TIA or minor stroke. The intervention will combine educational material and intensive HWC coaching.

The PERKS-International trial is coordinated by the Menzies Institute for Medical Research, University of Tasmania. The New Zealand arm of the study will be coordinated by NISAN.
It will be of four years duration and involve 790 participants aged >35 and ≤75 years, recruited across Australia and New Zealand. Participants will be followed for at least 12 months.
Study background and aim
Stroke is one of the biggest causes of death and disability in the world today which is affecting all ages, ethnicities, and socioeconomic groups. It carries an enormous emotional and socioeconomic impact on patients, families, and health services. However, many strokes are preventable, and its onset can be reduced simply by being aware of and controlling certain lifestyle factors.
The PERKS-International trial study compares two different ways of showing people their risk factors for stroke. We will test whether one method is better than the other at helping people to manage their stroke risk factors including diet, exercise and blood pressure.
Collaborators
- Associate Professor Seana Gall, Menzies Institute for Medical Research, University of Tasmania
- Professor Valery Feigin, National Institute for Stroke and Applied Neurosciences, Auckland University of Technology
- Professor Rita Krishnamurthi, National Institute for Stroke and Applied Neurosciences, Auckland University of Technology
- Professor Timothy Kleinig, Central Adelaide Local Health Network Incorporated, trading as Royal Adelaide Hospital
- Doctor Derrick Bennett, Clinical Trial Service Unit and Epidemiological Studies Unit, Nuffield Department of Population Health, University of Oxford
- Professor Amanda Thrift, Epidemiology and Prevention Division, Stroke and Ageing Research, Department of Medicine, School of Clinical Sciences at Monash Health, Monash University
- Professor Dominique Cadilhac, Translational Public Health and Evaluation Division, Stroke and Ageing Research, Department of Medicine, School of Clinical Sciences at Monash Health, Monash University
- Professor Mark Nelson, Discipline of General Practice, University of Tasmania
- Ms Tara Purvis , Translational Public Health and Evaluation Division, Stroke and Ageing Research, Department of Medicine, School of Clinical Sciences at Monash Health, Monash University
Timeline: 2021 - 2024
Funded by Australian National Health and Medical Research Council (Budget $790.000)
Contact: Rita Krishnamurthi or Research Study Manager Shabnam Jalili-Moghaddam
Developed in collaboration with international leaders in stroke prevention, the Stroke RiskometerTM app is an award winning and easy-to-use tool for measuring your individual risk of a stroke. The app is able to calculate your risk through evaluating a series of risk factors such as age, gender, ethnicity, lifestyle and other health factors that directly influence your likelihood of a stroke within the next five and ten years. It will supply essential information on how you can reduce your chance of having a stroke and will monitor your risk as you start to modify your personal risk factors.

TIA and minor stroke are at high risk of secondary vascular events including major stroke, myocardial infarction, cognitive deficits and death, as high as 25% within 90 days. Evidence suggests modifying health behaviours prevention is feasible, improves health outcomes, reduces healthcare costs, risk of stroke by about 80%, and stroke incidence about 50%. Health behaviours, lifestyle interventions, can lead to reductions in CVD and stroke. Health and wellness coaching (HWC) is a multidimensional intervention improving lifestyle and maintaining health and wellbeing. The main aim is to determine the effectiveness of HWC in improving blood pressure at 6 months post-randomisation and secondary aimsare to determine the impact of HWC on overall cardiovascular disease risk based on the LS7, use of the Stroke Riskometer app; quality of life; stroke awareness; cognition; medication adherence, adverse cardiovascular events, health service use and costs. Detect at least a 6 mm Hg clinically significant difference in systolic BP changes at 6 months from baseline, between the HWC and UC groups. Following screening for eligibility, consenting and the baseline assessment, participants will be randomised to Usual Care for HWC groups. Assessments are conducted at 3-, 6-, 9- and 12- months post-randomisation. The trial will determine HWC will lead to clinically meaningful improvements in lifestyle behaviours and reduce the risk for secondary vascular events including major stroke.
Design: A prospective, phase III, open-label, single-blinded end-point randomised controlled trial of 360 participants
Study population
The study aims to recruit 360 adults aged 18 years or older recently diagnosed with TIA or first-ever minor stroke (excluding subarachnoid haemorrhage (SAH)) with no or minor disabilities at discharge, and who are independent in activities of daily living. Eligible participants would be those:
- admitted to one of the three Auckland-based hospitals or identified via primary care for minor stroke or TIA
- have at least 2 modifiable risk factors (such as diabetes, high cholesterol, smoking, overweight)
- with systolic blood pressure either between 120-129 mm Hg and on blood pressure medications OR systolic blood pressure ≥130 mm Hg
- able to converse in English and provide written informed consent.
Collaborators
- Prof Valery Feigin - NISAN, AUT
- Prof Rita Krishnamurthi - NISAN, AUT
- Dr Irene Zeng - AUT
- Prof Suzanne Barker-Collo - The University of Auckland
- Prof Alan Barber - The University of Auckland
- Dr Braden Te Ao - The University of Auckland
- Dr Yogini Ratnasabapathy - Te Whatu Ora - health New Zealand, Waitemata
Timeline: 01 October 2022 - 30 September 2024
Funded by Health Research Council of New Zealand (Budget $450,000)
Contact
- Co-Principal Investigator Rita Krishnamurthi
- Study Manager Sulekha Devaki De Silva
- Programme Manager Bala Nair
- Research Officer Jesse Dyer
Stroke is the second most common cause of death and the third leading cause of disability in the world. Recurrent strokes and transient ischaemic attacks (TIA) contribute significantly to the overall burden of cardiovascular disease (CVD). About 20-25% of strokes occur in people with a previous stroke or transient ischemic attack (TIA), during 5 years of the index event. CVD events account for 50–70% of the deaths after stroke. Up to 90% of recurrent strokes and TIAs are potentially preventable with effective secondary stroke prevention. Despite this, no major improvements in stroke recurrence rates have been observed over the last three decades in New Zealand (NZ) or internationally.
This randomised controlled trial (RCT) aims to determine the efficacy and uptake of a web-app for clinicians combined with a mobile-app for secondary stroke prevention in adults (35-79 years) with TIA or IS.
The intervention
Participants will be randomised to either the intervention group (IG) or the usual care (UC) group using computerised block randomisation. IG subjects will be assessed by their hospital clinicians using the web-app; provided with their recurrent risk assessment results, personalised recommendations (including built-in motivational tools), and informed of the Stroke Riskometer mobile-app for self-management post-discharge. Those in UC will not have the web-app assessment, nor be informed of the mobile app.
Outcomes
The co-primary outcome will be a clinically significant reduction in systolic blood pressure and low-density lipid cholesterol in the IG group, compared to the UC group, at 6 months post-randomisation. Secondary aims include adherence to medications and recommended lifestyle behaviours, usability, potential for implementation and, cost effectiveness of the intervention.
Design
Randomised Controlled Trial
Inclusion criteria
- Adults aged 35-75 years with first-ever-in-a-lifetime stroke or TIA
- No significant cognitive impairment as measured by standard cognitive assessments
- No significant language issues preventing effective communication; and
- Access to a smartphone or tablet device
Investigators
- Professor Rita Krishnamurthi (Principal Investigator)
- Professor Valery Feigin
- Dr Yogini Ratnasabapathy
- Dr Karim Mahawish
- Dr Irene Zeng
- Dr Braden Te Ao
- Dr Bala Nair
- Dr Alexander Merkin
Project Manager
- Dr Shabnam Jalili-Moghaddam
Timeline
- 1 October 2023 - 30 September 2027
Recruitment start date
- 1 April 2024
Funded by
- Health Research Council of New Zealand (Budget $1.44million)
Contact
Professor Rita Krishnamurthi
Email: rita.krishnamurthi@aut.ac.nz
Phone: 09 921 9999 ext 7809
Completed projects
An epidemiological study of the determinants of stroke impact on individuals, families and communities, carried out in Auckland in 2002–2003.
Rationale
Stroke is the third leading cause of death in New Zealand, and a major cause of disability. It has an enormous impact on patients, carers and society. About 18,000 people are living with the effects of stroke in New Zealand. This number is projected to double by 2020. There is uncertainty about which key socioeconomic and health service factors in this country influence recovery from stroke. Moreover, there is little information about the access and quality of stroke services, in particular for Maori and Pacific people who are at high risk of stroke and who experience inequity in healthcare.
Aims
The overall aim of this study was to quantify the impact of stroke in Auckland, to refine methods for assessing this impact, and to identify whether factors such as socioeconomic circumstances, ethnicity, case mix, and quality of healthcare delivery, influence variations in impact.
Updates
- This study is now complete but the data analysis still continues. The major findings of this study to date are:
- A trend towards declining stroke incidence rates in New Zealand Europeans over the last 20 years, while in the same period Maori and Pacific populations have shown a near doubling of stroke incidence.
- In Maori and Pacific people, strokes occur at a younger age – on average up to 10 and 15 years earlier than in New Zealand Europeans.
- New Zealand Europeans experience less severe strokes than other ethnic groups in NZ.
- Compared to New Zealand Europeans, Maori, Pacific Islanders and Asian people are at 1.5 to 3 times’ greater risk of ischaemic stroke and intracerebral haemorrhage.
- The increased risk of stroke in Maori, Pacific Islanders and Asian people is partly attributed to a higher prevalence of obesity, diabetes and high blood pressure in these ethnic groups.
Design
The study created a prospective population-based stroke register for the total population of Auckland in 2002–2003. Survivors of all new cases of stroke over a 12-month period were subsequently followed for the next six months. The methodology included similar criteria for diagnosis, case ascertainment, outcomes, and reporting to the criteria that were well established in previous studies of stroke in Auckland (initially 680 patients identified in 1981–82, and then 1761 patients identified in 1991–92). In addition, the study used both qualitative and quantitative measures to determine the impact of stroke. Data processing and analyses were undertaken within the CTRU.
Collaborators
AUT Investigators
- Valery Feigin, Co-Principal Investigator
- Elizabeth Mitchelson, Named Investigator
Co-Collaborators
- Craig Anderson, Principal Investigator (The George Institute for International Health, Sydney, Australia)
- Derrick Bennett, Named Investigator (University of Oxford, United Kingdom)
- Alan Barber, Named Investigator (Department of Medicine, The University of Auckland)
- Ruth Bonita, Named Investigator (Non-Communicable Disease Surveillance, World Health Organization, Geneva, Switzerland)
- Paul M Brown, Named Investigator (Department of Community Health, The University of Auckland)
- Lorna Dyall, Named Investigator (Department of Community Health, The University of Auckland)
- Sitaleki Finau, Named Investigator (Maori and Pacific Health, The University of Auckland)
- Ngaire Kerse, Named Investigator (Department of General Practice and Primary Health Care, The University of Auckland)
- Harry McNaughton, Named Investigator (Wellington School of Medicine)
- Malakai Ofanoa, Named Investigator (Maori and Pacific Health, The University of Auckland)
- Joe Singh, Named Investigator (North Shore Hospital, Auckland)
- Alistair Woodward, Chair of Steering Committee (School of Population Health, The University of Auckland)
The study is funded by the Health Research Council of New Zealand.

Stroke is the second leading cause of death and disability worldwide. The absolute numbers of people having stroke has increased in New Zealand (NZ) and worldwide mainly due to increasing and ageing populations. Patients with transient ischaemic attack (TIA) are at a high risk of secondary vascular events including major stroke, myocardial infarction (MI), cognitive deficits and death, with population-based studies reporting incidence of adverse outcomes as high as 25% within 90 days. In NZ, there are about 9,000 new strokes and 3,000 new TIAs each year, with direct annual costs estimated at >$650 million to the health sector. Understanding the cost burden of stroke from a societal perspective is essential for resource allocation.
The Auckland Regional Community Stroke Studies (ARCOS) are internationally recognised as ideal population-based registers of stroke incidence and outcomes which have been conducted in NZ every decade since 1981. ARCOS studies have shown that while both stroke incidence and mortality rates had declined over the previous 30 years, the incidence of stroke in NZ continues to be among the highest in developed countries. The ARCOS V study consists of three inter-linked objectives to provide the most recent and up-to-date evidence-base for measuring stroke burden in New Zealand. This will be the fifth ARCOS study in the ARCOS series, with the overarching aim to reliably determine trends in stroke incidence, prevalence and outcomes for a fifth 10-year time point.
Accurate and representative population-based data are also crucial to: (1) determine the true incidence, causes and outcome of stroke; (2) evidence-based health care planning, across the care spectrum; (3) evaluating the need for and impact of preventative/management strategies; (4) address persistent uncertainty about what key factors (socioeconomic & health service) impact stroke recovery in NZ; (5) examine the natural course of recovery, particular for cognitive and behavioural outcomes; (6) provide information on access and satisfaction with stroke services, especially for Māori and Pacific people who are at high risk of stroke and face inequities in health care accessing; and (7) identify service gaps/unmet needs to ensuring evidence-based policy, resource allocation, prevention planning, management services, and evaluation of service performance.
Collaborators
- Professor Valery Feigin, AUT
- Dr Rita Krishnamurthi, AUT
- Professor Suzanne Barker-Collo, University of Auckland
- Dr Priya Parmar, AUT
- Professor Alan Barber, University of Auckland
- Dr Susan Maohn, AUT
- Dr Hinemoa Elder,Te Wānanga o Aotearoa
- Professor Bruce Arroll, University of Auckland
- Dr Yogini Ratnasabapathy, Waitemata District Health Board
- Associate Professor Annemarei Ranta, University of Otago
Timeline: September 2020 - December 2021
Funded by Health Research Council of New Zealand (Budget $1.2million)
Contact: Rita Krishnamurthi or ARCOS Team or Study Manager Bala Nair
A second component of the ARCOS IV study, Motivational Interviewing Stroke Trial (MIST), is to evaluate a novel, potentially widely applicable behavioural intervention to reduce stroke recurrence. The goal of this intervention is to prevent a second stroke with clients. We aim to do this by giving clients a forum in which to discuss their physicians' recommendations (such as medications, physical activity and diet) as well as their overall health. All topics are open for discussion because we understand that many areas of life connect to health and happiness.
Contact: Rita Krishnamurthi
Stroke is a major cause of death and disability worldwide, yet 90% of strokes can be prevented by adequate control of modifiable risk factors (e.g. high blood pressure, diabetes, smoking) through lifestyle modifications and medications. Individuals at a high risk of stroke can be identified by their family doctor through a cardiovascular disease risk calculator (PREDICT).
Those at a high 5-year risk should be prescribed medications and/or given recommendations to lifestyle changes to reduce cardiovascular risk. However, adherence to these recommendations is low, resulting in preventable strokes. Health/Wellness Coaching is a psychological intervention that may enhance adherence to doctor’s recommendations, and reduce stroke risk.
This study aims to determine the feasibility of a planned randomised clinical trial to test the effectiveness of health/wellness coaching for the primary prevention of stroke and cardiovascular disease in the community.
Aims
The aim of the study is to help identify any issues that need to be addressed before commencing a full scale randomised clinical trial to test the effectiveness of Health and Wellness Coaching (HWC) in reducing the risk of stroke and cardiovascular disease in the community.
Design
This study is a phase II, open label, single centre randomised control trial (n=24) addressing feasibility issues of HWC coaching for primary stroke prevention in high stroke and CVD risk subjects to inform the design and methodology of statistically powered phase III randomised controlled trial.
Outcome measures
The main outcome of the study will be feasibility of screening for eligible participants at primary healthcare practices in Auckland, rate of recruitment, rate of retention in the study and level of completion of case record forms and feedback from study participants. Relevant information to be collected in the full trial such as demographic information and other relevant medical information will be recorded for each study participant. To assess behaviour modification, each study participant will complete questions on general health and lifestyle information such as smoking status, diet, exercise, and medications during the phone interview at baseline and 3 months after the randomisation.
Contact: Rita Krishnamurthi
This study is a collaborative international project involving individual participant, stroke, and environmental data to determine if environmental factors such as weather, air pollution and geomagnetic activity can trigger the occurrence of stroke.
Evidence is being assessed from individual participant data meta-analysis of 11,157 patients from population-based stroke incidence studies in New Zealand, Australia (two centres), United Kingdom, France, and Sweden.
The International Stroke Incidence Studies Data Pooling Project collaborators are:
- Baker Heart Research Institute, National Stroke Research Institute, and Department of Epidemiology and Preventive Medicine, Monash University, Melbourne, Australia Neurological & Mental Health Division, George Institute for International Health, University of Sydney, Australia
- Service de Neurologie, Centre Hospitalo-Universitaire, Dijon, France
- The National Institute for Stroke and Applied Neurosciences, AUT, Auckland, New Zealand
- The Clinical Trials Research Unit and Department of Statistics, University of Auckland, New Zealand
- Department of Public Health and Clinical Medicine, Umeå University, Umeå, Sweden
- University Department of Clinical Neurology, University of Oxford, Oxford, United Kingdom
Contact: Valery Feigin
Subarachnoid haemorrhage (SAH) accounts for 1-7% of all strokes. Outcome may be poor with a mortality rate of 33-45% within 30 days, and survivors often having permanent disabilities that significantly interfere with daily activities.
Significant new management strategies have been introduced over the last 30 years, and selective coiling of aneurysms is now available for certain aneurysm patients. The impact of the implementation of these changes in practice, and its effect on outcomes at a population level are unknown.
The study will use the internationally unique longitudinal population-based stroke data (ARCOS) to determine whether changes in SAH management over the past three decades have influenced patient outcomes in New Zealand (NZ). This study will provide information about the effectiveness of current practices, identify gaps in the management, and determine predictors of better outcomes of SAH for health professionals.
Funded by the Faculty of Health & Environmental Sciences, AUT University and the Neurological Foundation.
Collaborators
- Ms Flora Suh
- Dr Rita Krishnamurthi
- Mr Steve Taylor
- Dr Patrick Schweder
- Prof. Kathryn McPherson
- Assoc. Prof. Suzanne Barker-Collo
- Prof. Alan Barber
- Mr Edward Mee
- Professor Valery Feigin
Contact: Rita Krishnamurthi
A prospective longitudinal study of long-term (5 to 6-year) stroke outcomes (neuropsychological impairment, impairment, disability, handicap, HRQoL, and survival).
The study sourced its participants and utilised existing baseline, 6-month and 1-year follow-up data from the population-based stroke incidence study carried out in Auckland in 2002-2003.
Comprehensive neuropsychological measurements combined with all major domains of functional outcome measurements (disability, handicap and HRQoL) in the large study sample of long-term (5 to 6-year) stroke survivors with well CT/MRI verified stroke subtypes were the most unique features of this study.
Over 500 stroke survivors and their informal caregivers previously have been enrolled in the study.
Study data collection was completed in May 2009.
Collaborators
- V Feigin (AUT)
- S Barker-Collo (Auckland University)
- H Senior (Auckland University)
- CMM Lawes (Auckland University)
- V Parag (Auckland University)
- P Brown (Auckland University)
An epidemiological study of the determinants of stroke impact on individuals, families and communities, carried out in Auckland in 2002–2003.
Stroke is the third leading cause of death in New Zealand, and a major cause of disability. It has an enormous impact on patients, carers and society. About 18,000 people are living with the effects of stroke in New Zealand. This number is projected to double by 2020. There is uncertainty about which key socioeconomic and health service factors in this country influence recovery from stroke. Moreover, there is little information about the access and quality of stroke services, in particular for Maori and Pacific people who are at high risk of stroke and who experience inequity in healthcare.
Aims
The overall aim of this study was to quantify the impact of stroke in Auckland, to refine methods for assessing this impact, and to identify whether factors such as socioeconomic circumstances, ethnicity, case mix, and quality of healthcare delivery, influence variations in impact.
Updates
- This study is now complete but the data analysis still continues. The major findings of this study to date are:
- A trend towards declining stroke incidence rates in New Zealand Europeans over the last 20 years, while in the same period Maori and Pacific populations have shown a near doubling of stroke incidence.
- In Maori and Pacific people, strokes occur at a younger age – on average up to 10 and 15 years earlier than in New Zealand Europeans.
- New Zealand Europeans experience less severe strokes than other ethnic groups in NZ.
- Compared to New Zealand Europeans, Maori, Pacific Islanders and Asian people are at 1.5 to 3 times’ greater risk of ischaemic stroke and intracerebral haemorrhage.
- The increased risk of stroke in Maori, Pacific Islanders and Asian people is partly attributed to a higher prevalence of obesity, diabetes and high blood pressure in these ethnic groups.
Design
The study created a prospective population-based stroke register for the total population of Auckland in 2002–2003. Survivors of all new cases of stroke over a 12-month period were subsequently followed for the next six months. The methodology included similar criteria for diagnosis, case ascertainment, outcomes, and reporting to the criteria that were well established in previous studies of stroke in Auckland (initially 680 patients identified in 1981–82, and then 1761 patients identified in 1991–92). In addition, the study used both qualitative and quantitative measures to determine the impact of stroke. Data processing and analyses were undertaken within the CTRU.
Collaborators
AUT Investigators
- Valery Feigin, Co-Principal Investigator
- Elizabeth Mitchelson, Named Investigator
Collaborators
- Craig Anderson, Principal Investigator (The George Institute for International Health, Sydney, Australia)
- Derrick Bennett, Named Investigator (University of Oxford, United Kingdom)
- Alan Barber, Named Investigator (Department of Medicine, The University of Auckland)
- Ruth Bonita, Named Investigator (Non-Communicable Disease Surveillance, World Health Organization, Geneva, Switzerland)
- Paul M Brown, Named Investigator (Department of Community Health, The University of Auckland)
- Lorna Dyall, Named Investigator (Department of Community Health, The University of Auckland)
- Sitaleki Finau, Named Investigator (Maori and Pacific Health, The University of Auckland)
- Ngaire Kerse, Named Investigator (Department of General Practice and Primary Health Care, The University of Auckland)
- Harry McNaughton, Named Investigator (Wellington School of Medicine)
- Malakai Ofanoa, Named Investigator (Maori and Pacific Health, The University of Auckland)
- Joe Singh, Named Investigator (North Shore Hospital, Auckland)
- Alistair Woodward, Chair of Steering Committee (School of Population Health, The University of Auckland)
The study is funded by the Health Research Council of New Zealand.
Journal articles
- Theadom, A., Rutherford, S., Kent, B., & McPherson, K. (in press 2018). The process of adjustment over time following stroke: A longitudinal qualitative study. Neuropsychological Rehabilitation, pp. 1-11. doi:10.1080/09602011.2018.1440609
- Phan, H.T., Blizzard, C.L., Mathew, J., Reeves, M.J., Thrift, A.G., Cadilhac, D.A., ... Gall, S.L. (in press 2018). Factors contributing to sex differences in functional outcomes and participation after stroke. Neurology.
- Krishnamurthi R.V. Barker-Collo, S., Parag, V., Parmar, P., Witt, E., Jones, A., .... Feigin, V.L. (2018). Stroke incidence by major pathological type and ischaemic subtypes in the Auckland Regional Community Stroke Studies. Stroke, 49(1), doi:10.1161/STROKEAHA.117.019358
- Phan, H. T., Blizzard, C. L., Reeves, M. J., Thrift, A. G., Cadilhac, D., Sturm, J., . . . Gall, S. (2017). Sex differences in long-term mortality after stroke in the INSTRUCT (INternational STRoke oUtComes sTudy): A meta-analysis of individual participant data. Circulation: Cardiovascular Quality and Outcomes, 10(2). doi:10.1161/CIRCOUTCOMES.116.003436
- Mahon, S., Parmar, P., Barker-Collo, S., Krishnamurthi, R., Jones, K., Theadom, A., & Feigin, V. L. (2017). Determinants, prevalence and trajectory of long-term post stroke cognitive impairment: Results from 4-year follow-up of the ARCOS-IV Study. Neuroepidemiology, 49(3-4), 129-134. doi:10.1159/000484606
- Barker-Collo, S., Krishnamurthi, R., Witt, E., Theadom, A., Starkey, N., Barber, P. A., . . . Feigin, V. (2017). Depression and anxiety across the first year after Ischemic stroke: Findings from a population-based New Zealand ARCOS-IV study. Brain Impairment, 18(3), 265-276. doi:10.1017/BrImp.2017.12
- Barker-Collo, S., Krishnamurthi, R., Feigin, V., Jones, A., Theadom, A., Barber, P. A., . . . Bennett, D. (2016). Neuropsychological outcome and its predictors across the first year after ischaemic stroke. Brain Impairment, 17(2), 111-122.
- Barber, P. A., Krishnamurthi, R., Parag, V., Anderson, N. E., Ranta, A., Klifoyle, D., . . . for the ARCOS IV study group. (2016). Incidence of transient ischemic attack in Auckland, New Zealand, in 2011 to 2012. Stroke, 47(9), 2183-2188. doi:10.1161/STROKEAHA.116.014010
- Barker-Collo, S., Krishnamurthi, R., Witt, E., Feigin, V. L., Jones, A., McPherson, K., . . . Arroll, B. (2015). Improving adherence to secondary stroke prevention strategies through motivational interviewing. Stroke, 46(12), 3451-3458. doi:10.1161/STROKEAHA.115.011003
- Feigin, V. L., Krishnamurthi, R. V., Barker-Collo, S., McPherson, K. M., Barber, P. A., Parag, V., . . . ARCOS IV Group. (2015). 30-year trends in stroke rates and outcome in Auckland, New Zealand (1981-2012): A multi-ethnic population-based series of studies. PLoS One, 10(8), 1-30. doi:10.1371/journal.pone.0134609
- Krishnamurthi, R., Witt, E., Barker-Collo, S., McPherson, K., Davis-Martin, K., Bennett, D., . . . ARCOS IV Programme Group. (2014). Reducing recurrent stroke: Methodology of the motivational interviewing in stroke (MIST) randomized clinical trial. International Journal of Stroke, 9(1), 133-139. doi:10.1111/ijs.12107
- Krishnamurthi, R., Jones, A., Barber, P. A., Barker-Collo, S., McPherson, K., Bennett, D., . . . ARCOS IV Programme Group. (2014). Methodology of a population-based stroke and TIA incidence and outcomes study: The Auckland Regional Community Stroke Study (ARCOS IV) 2011-2012. International Journal of Stroke, 9(1), 140-147. doi:10.1111/ijs.12108
- Kasabov, N., Feigin, V., Hou, Z. -G., Chen, Y., Liang, L., Krishnamurthi, R., . . . Parmar, P. (2014). Evolving spiking neural networks for personalised modelling, classification and prediction of spatio-temporal patterns with a case study on stroke. Neurocomputing, 134, 269-279. doi:10.1016/j.neucom.2013.09.049
- Rutherford, S. J., Theadom, A., Jones, A., Hocking, C., Feigin, V., Krishnamurthi, R., . . . Mcpherson, K. M. (2014). Capturing the stories behind the numbers: The Auckland Regional Community Stroke study (ARCOS IV), a qualitative study. International Journal of Stroke, 9(1), 64-70. doi:10.1111/ijs.12164
Conference abstracts
- Mahon S., Krishnamurthi, R., Jones, K., Parmar, P., Barker-Collo, S., & Feigin, V. (2017). Long-term neuropsychological impairment in 4 year stroke survivors. In 46th Annual Meeting of the International Neuropsychological Society. Washington D.C., USA. Retrieved from https://www.the-ins.org/meeting/future-ins-meetings/ins-washington-dc-2018/
- Mahon S., Krishnamurthi, R., Jones, K., Feigin, V., Parmar, P., & Witt, E. (2017). Long-term cognitive impairment following stroke: Results from the 3-year ARCOS IV follow-up study. In 3rd European Stroke Organisation Conference. Prague, Czech Republic. Retrieved from http://www.esoc2017.com/
- Tunnage, B., Krishnamurthi, R. V., Feigin, V., & Swain, A. (2017). Identifying the first medical contact in acute stroke and TIA: A population-based study. In 27th Annual Scientific Meeting of the Stroke Society of Australasia 2017. International Journal of Stroke Vol. 12 (pp. 3-59). Queenstown, New Zealand. doi:10.1177/1747493017720548
- Zagreanu, C., Krishnamurthi, R. et.al. (2017). Epidemiology of atrial fibrillation in ischemic stroke patients: A population-based study in Auckland, New Zealand. International Journal of Stroke, 12(3), 3-59.
- Mahon, S. (2016). Long-term impact of stroke on cognition. In New Zealand Applied Neurosciences Conference. Neuroepidemiology, 47 (pp. 142). Auckland, New Zealand. doi:10.1159/000453097
- Mahon, S. (2015). 3-year stroke survivors: The long-term impact of stroke on cognition and factors associated with recovery. In Combined 26th ASM of the Stroke Society of Australasia and the 11th Australasian Nursing and Allied Health Stroke Conference (SMART Strokes). International Journal of Stroke, 10(S3) (pp. 6-7). Melbourne, Australia.
- Curran, A., Jones, A. R., Krishnamurthi, R., Barker-Collo, S., McPherson, K., & Feigin, V. L. (2015). Prevalence of smoking in stroke patients and its relationship with stroke severity. International Journal of Stroke, 10, 66.
- Barber, P. A., Krishnamurthi, R., Parag, V., Anderson, N. E., Ranta, A., Kilfoyle, D., . . . Feigin, V. L. (2015). Incidence and attack rates of stroke and transient ischaemic attack in Auckland, New Zealand, in 2011-2012. International Journal of Stroke, 10, 202.
- Jones, A. R., Krishnamurthi, R., Theadom, A., Barker-Collo, S., McPherson, K., & Feigin, V. L. (2015). Health-related quality of life in stroke survivors one year post stroke. International Journal of Stroke, 10, 66.
- Feigin, V. L., Krishnamurthi, R., Barker-Collo, S., McPherson, K., Parag, V., Abbott, M., . . . Barber, A. P. (2014). Long-term trends in stroke incidence in New Zealand: 1981-2012. International Journal of Stroke, 9(3), 153.
- Krishnamurthi, R., Barker-Collo, S., McPherson, K., Parag, V., Rush, E., Davis-Martin, K., . . . Feigin, V. (2014). Incidence and outcomes of stroke: Findings from the population-based Auckland Regional Community Stroke Study (ARCOS IV). In 25th Annual Scientific Meeting of the Stroke Society of Australasia. Queensland, Australia. International Journal of Stroke, 9(S1), 12.
- Bhattacharjee, R., Krishnamurthi, R., Barker-Collo, S., McPherson, K., Parmar, P., Rush, E., . . . Witt, E. (2014). Stroke incidence in younger adults from Auckland, New Zealand: Findings from the ARCOS IV Stroke study. In 25th Annual Scientific Meeting of the Stroke Society of Australasia. International Journal of Stroke, 9(S1), 12-13.Queensland, Australia.
- Krishnamurthi, R., Jones, A., Feigin, V. L., Barker-Collo, S., McPherson, K., Barber, P. A., & on behalf of the ARCOS IV Programme Group. (2013). Incidence and outcomes of TIA: Preliminary findings from the population-based Auckland Transient Ischemic Attack Study (ATIAS). In 24th Annual Scientific Meeting of the Stroke Society of Australasia. Darwin, Australia: International Journal of Stroke 8(S1), 11-26.
- Suh, F. M., Krishnamurthi, R., Schweder, P., Taylor, S., McPherson, K., Barker-Collo, S., . . . Feigin, V. (2013). Temporal changes in management and outcomes of subarachnoid haemorrhage: Trends over 30 years. In 24th Annual Scientific Meeting of the Stroke Society of Australasia. Darwin, Australia: International Journal of Stroke 8(S1), 11-26.
- Krishnamurthi, R., Jones, A., Barker-Collo, S., McPherson, K., Feigin, V., & the ARCOS IV Programme Group. (2012). ARCOS IV: Stroke Incidence and outcomes. In V. L. Feigin, & M. Giroud (Eds.), 2nd International Congress of Neurology and Epidemiology. Nice, France: Neuroepidemiology 39(3-4), 212-212. doi:10.1159/000343765
PhD thesis
- Tunnage B (Completed 2018)
- Kalaga H (Submitted 2018)
Cardiovascular disease is NZ's biggest killer and leading cause of loss of healthy life years. Maori are disproportionately affected and cardiovascular disease is the main reason for the increasing difference in life expectancy between Maori and non Maori. Reducing cardiovascular disease and removing these inequalities will require extensive public health strategies.
One approach, which could achieve substantial benefits within a few years, is fixed-dose combination medication (a "polypill"). The polypill has the potential to address the current treatment gap for individuals at high risk of cardiovascular disease, and to improve the utilisation of long-term preventive therapies consistent with guideline recommendations.
Aims
The primary aim of the study is to assess whether provision of combination cardiovascular medication (a "polypill") compared to continuing usual cardiovascular medications improves clinical outcomes in high-risk patients by increasing adherence to guideline recommended therapy; and to assess whether results are similar for Maori and non-Maori.
Design
This is an open label, randomised, controlled trial. 600 participants (including 300 Maori) at high risk of cardiovascular disease will be recruited through primary care. Participants will be randomised to the polypill (containing low dose aspirin, a statin and two blood pressure lowering medicines) or to usual care (cardiovascular medication as prescribed by their general practitioner) and followed for one year. The primary outcomes are adherence, and change in blood pressure and cholesterol levels.
CTRU Investigators
- Anthony Rodgers, Principal Investigator
- Valery Feigin
- Natasha Rafter
- Vanessa Selak
- Stephen Vander Hoorn
- Puti Wilson
Collaborators
- Bruce Arroll, General Practice & Primary Health Care, University of Auckland;
- Dale Bramley, Waitemata DHB;
- Jennie Connor, Rod Jackson, and Richard Milne, Epidemiology & Biostatistics, University of Auckland;
- Rob Cook, Bazian Ltd, London, UK;
- Sue Crengle, Maori Health, University of Auckland;
- Rob Doughty, Auckland DHB;
- Tim Maling, Capital & Coast DHB;
- Bruce Neal, The George Institute for International Health, Sydney, Australia;
- Anushka Patel, The George Institute for International Health, Sydney, Australia;
- David Simmons, Institute of Metabolic Sciences, University of Cambridge, UK.
Funded by Health Research Council of New Zealand
Hypothesis
- That the incidence of transient ischemic attack (TIA) in Auckland is higher than other developed countries.
- That the risk of stroke and cardiovascular disease following TIA in Auckland is greater than other developed countries.
- That the ABCD2 stroke risk stratification score is less accurate at predicting adverse outcomes than originally reported.
Aim
- To determine the community-based incidence, outcome and risk factor profile of TIA in an ethnically mixed population.
- To determine the accuracy of the ABCD2 stroke risk stratification score in a general practice, emergency department and specialist TIA clinic, and whether it requires modification.
TIA can be simply defined as stroke-like symptoms and signs that resolve within 24 hours. About 25% of people with ischemic stroke have a preceding or warning TIA. Recent evidence highlights that the risk of stroke following TIA is greatest in the first 48 hours but may still be as high as 10% at 30 days and 20% at 90 days. Studies have shown that this risk of stroke can be reduced by up to 80% by rapid assessment, investigation and commencement of secondary prevention measures.
There have been few population based studies of the incidence and outcome of TIA. Most of these studies were performed over 10 years ago before there was widespread use of medications to lower cholesterol levels and blood pressure low and surgical intervention in patients with internal carotid artery stenosis. Even fewer TIA studies have looked at the effect of ethnicity on incidence and outcome.
We will test the hypotheses that the incidence of TIA is higher, and the outcome is worse, in Auckland than in other developed countries, and this may be explained by differences in our ethnically diverse population. We will also examine the accuracy of the ABCD2 stroke risk stratification score and determine if it should still be recommended in national and international stroke and TIA guidelines, or if (and how) it should be modified.
We will identify all patients with TIA between 1st March 2011 and 28th February 2012 who are aged 15 years or older and resident in Auckland, including those patients presenting to hospital or who are managed in the community. The patient identification processes of the fourth Auckland Regional Community Stroke study (ARCOS IV) will be utilised. All participants will be assessed at day 90 and 12 months.
Crude and age, ethnic, and sex standardized TIA incidence (first-ever events) and attack (all events) rates of stroke per 100 000 people will be determined. The incidence of stroke and other adverse cardiovascular events at 48 hours, 7 days, 90 days and 12 months will be determined. The ability of the ABCD2 score to discriminate between those who go on to have a stroke and those who do not, will also be determined.
This study has a high potential to play a central role in the planning of services and development of health policy in relation to TIA and stroke, within New Zealand and internationally, and be used to inform evidence-based recommendations for health care.
ATIAS concluded in September 2013.
Collaborators
- Professor Alan Barber (Principle Investigator)
- Prof Valery L Feigin
- Dr Neil E Anderson
- Dr Dean K Kilfoyle
- Dr Edward Wong
- Dr Rita V Krishnamurthi
Funding
- The Auckland Medical Research Fund, and
- The New Zealand Neurological Foundation
Contact: Rita Krishnamurthi
Changing behaviour to reduce stroke risk using the Stroke RiskometerTM mobile app – a pilot randomised control trial
Stroke is a devastating yet highly preventable disease. There are about 9000 strokes every year in New Zealand, 30% of which are fatal in the first year and a further 70% of survivors are left with some level of disability. There is evidence that modifying health behaviours is feasible, improves health outcomes, reduces healthcare costs and can reduce an individual’s risk of stroke by about 80%.
However, the level of public awareness of stroke, its risk factors, and how to manage them is low, particularly in communities with low socioeconomic status, in ethnic minority groups and in rural areas. In addition, current high-risk CVD prevention strategies do not target people with low to moderate risk of CVD, which is where the majority of strokes and heart attacks arise.
There is accumulating evidence of the feasibility and effectiveness of using mobile technologies for improving health. The increasing burden of stroke suggests that current primary prevention strategies (’business as usual”) are not sufficiently effective. This highlights the need for an accurate and user-friendly tool to enable individuals to evaluate their own stroke risk, motivate them to reduce their risk and have access to the knowledge to manage their risk, with built-in feedback and the ability to monitor progress.
Aims
The aim of the study is to conduct a pilot trial to test the efficacy of the Stroke RiskometerTM app as a standalone and add-on tool for health behaviour modification and stroke education for the primary prevention of stroke. In addition, the study will inform on feasibility issues of conducting a full-scale trial, such as recruitment, acceptability of the intervention and sample size calculation for a full-scale trial to evaluate effectiveness of the app-based intervention, including cost-effectiveness evaluation, for the primary prevention of stroke.
Project tool place over 2 years, starting 1 March 2016.
Collaborators
- Valery Feigin, AUT, Auckland
- Suzanne Barker-Collo, The University of Auckland
- Rita Krishnamurthi, AUT, Auckland
- Leigh Hale, The University of Otago, Dunedin
- Debra Waters, The University of Otago, Dunedin
- Denise Wilson, AUT, Auckland
- Alice Theadom, AUT, Auckland
- Bruce Arroll, The University of Auckland, Auckland
- Ngaire Kerse, The University of Auckland, Auckland
- Alan Barber. The University of Auckland, Auckland
- Lynette Tippet,The University of Auckland, Auckland
- Yogini Rathnasabapathy, Waitemata District Health Board
- Peter Sandiford, Waitemata District Health Board
- Gerry Devlin, The NZ Heart Foundation
- Kevin Sheehy, Navigator Healthcare
Funded by Brain Research New Zealand - A Centre of Research Excellence:
- BRNZ brings together 67 research groups spread all over New Zealand. Our collaborative community-focused approach is unprecedented for research in New Zealand.
- We are striving to unlock the secrets of the ageing brain and producing a seismic shift in how researchers, clinicians and community groups partner together.
- Find out more about our interventions and treatments for neurodegenerative disorders of the ageing brain; such as Dementia, Stroke, Parkinson's Disease, Alzheimer's Disease and Huntington's Disease.
- When we share and collaborate in order to improve health outcomes for older people, the outcome is a healthier and happier New Zealand.
Recent studies have shown that knowledge of stroke and dementia risk factors and warning signs is deficient.
Despite compelling evidence that increasing population/country-specific knowledge about warning signs and risk factors can reduce stroke and dementia burden in the population, there has been no recent research on the prevalence and risk factors of stroke and dementia in NZ. Therefore this study aims to fill these gaps in knowledge by utilising two methods to determine
- stroke/dementia awareness, and
- prevalence of stroke/dementia and their risk factors in the NZ population.
Aims
- to develop and test a questionnaire about knowledge and awareness about stroke/dementia and their symptoms in Māori, Pasifika, Asian, and NZ Europeans aged 20+ to be used in the main survey (subject to a separate application to and funding from HRC in 2015); and
- to provide population estimates of stroke and dementia prevalence and risk factors in NZ adults (aged 20+). Secondary aim: to identify differences in prevalence of stroke and dementia and their risk factors among major demographic groups categorised by age, gender, and ethnicity. People younger than 20 years will not be included in this project as their risk profile for stroke and dementia is significantly different from that in adults.
Methods
The project will have two distinct but inter-linked studies to be conducted concurrently:
- A pilot nation-wide stroke/dementia awareness survey. A pilot questionnaire will be developed to determine stroke and dementia awareness in the NZ population. A national random sample of 400 adults stratified by ethnicity (100 Māori, 100 Pasifika, 100 Asian/other, and 100 NZ Europeans) aged 20 years and older will be surveyed using computer-assisted telephone interviewing (CATI), validated for CVD risk factor assessment in ethnically diverse populations.
- A nation-wide smartphone-based stroke/dementia cross-sectional study to determine the prevalence of stroke/dementia and their risk factors. The stroke/dementia awareness pilot survey will include a stratified sample across all major ethnic groups and all adults in New Zealand and capture information on awareness that will not be obtained from the Smartphone study. It may capture some populations that may not participate in the Smartphone based study for stroke/dementia prevalence (for e.g. Smartphones less likely to be used by the elderly). Therefore the two studies will provide both unique and complementary information on of stroke/dementia (1) awareness, and (2) prevalence.
Research impact
Data from this project is urgently needed in NZ to develop evidence-based and cost-effective interventions for primary prevention and management at the population level. A reliable national survey data will also assist knowledge transfer to policy makers; programme planners and funding agencies to make informed decisions about effective ways to promote healthy lifestyles that reduce the risk of stroke/dementia.
The project took place over two years, starting January 2015.
Collaborators
- Prof Valery Feigin, AUT, Auckland
- Assoc Prof Suzanne Barker-Collo, University of Auckland, Auckland
- Assoc Prof Lynette Joy Tippett, University of Auckland, Auckland
- Prof Alan Barber, University of Auckland, Auckland
- Prof John Dalrymple-Alford, University of Canterbury, Christchurch
- Prof. Richie Poulton, University of Otago, Dunedin
- Dr Nicholas J. Cutfield, University of Otago, Dunedin
- Dr Rita Krishnamurthi, AUT, Auckland
- Assoc Prof Chris Bullen, AUT, Auckland
- Prof Patria Hume, AUT, Auckland
- Dr Amy Jones, AUT, Auckland
- Rohit Bhattacharjee, AUT, Auckland
- Priya Parmar, AUT, Auckland
Funded by
- Brain Research New Zealand
- Auckland University of Technology, Auckland, New Zealand
Contact: Rita Krishnamurthi
Health and Wellness Coaching (HWC) for primary stroke and CVD prevention: a randomised control trial.
Aiming to determine the effectiveness of HWC for primary stroke prevention in Māori, Pasifika, Asians and NZ Europeans.
Strokes are the main cause of disease burden in older adults, yet evidence suggests more than 80% of strokes are preventable, with adequate control of modifiable risk factors. This proposal to test the effectiveness of Health and Wellness Coaching (HWC) for primary prevention of stroke, is particularly relevant to the ageing population where most strokes occur.
HWC is an innovative, structured, patient-focused multi-dimensional psychological intervention designed to motivate participants to adhere to recommended medication and lifestyle changes. This randomised control trial is being conducted in NZ to address the question: is HWC effective for primary stroke and CVD prevention in Māori, Pasifika, Asians and NZ Europeans? The primary outcome is a substantial relative risk reduction of CVD.
Collaborators
- Valery Feigin, AUT, Auckland
- Alan Barber, The University of Auckland, Auckland
- Elaine Rush, AUT, Auckland
- Rita Krishnamurthi, AUT, Auckland
- Bruce Arroll, The University of Auckland, Auckland
- Suzanne Barker-Collo, The University of Auckland, Auckland
- Alain Vandal, AUT, Auckland
- Priya Parmar, AUT, Auckland
- Himenoa Elder, Te Whare Wānanga o Awanuiārangi
- Alice Theadom, AUT, Auckland
- Paul Brown, AUT, Auckland
The project took place from November 2015 to July 2019.
Funded by
- The Ministry of Business, Innovation & Employment - National Science Challenges, Ageing Well.
- Research objective – to harness science to sustain health and wellbeing into the later years of life.
Contact: Susan Mahon or Rita Krishnamurthi
E-research Programme to measure and reduce the burden of major non-communicable disorders in the world.
The overarching research objective of this e-health research programme is to develop a smartphone and information technology platform for medical informatics that allows not only collection and storage of reliable epidemiological data about prevelence and determinants of NCD, but also the utilisation of the technology platforms for reducing the burden of these NCD in NZ and internationally. This particular application is to extend the capability of the AUT Stroke Riskometer App and associated AUT IT system to allow e-research data collection.
Based on information collected and completed studies, findings will be used to refine and extend the Stroke Riskometer algorithm in terms of its accuracy and applicability to different populations, and to develop new, evidence-based Apps for the prediction / prevention and management of major NCD in the world.
View video about the Stroke Riskometer App
Funded by AUT Strategic Research Investment Fund 2014.
Contact: Rita Krishnamurthi
Stroke is a leading cause of death in the world and a major cause of long-term adult disability. The emotional and socioeconomic impact of stroke on patients, families, and health services is enormous. However, the availability of community rehabilitation after hospital discharge is limited. Given the increasing number of stroke survivors, there is an urgent need to develop alternatives to costly face-to-face therapist rehabilitation to support stroke survivors and their families.
One strategy is to maximise the benefits of new technologies, such as instructional DVDs and app development. Professor Valery Feigin and colleagues have developed a novel, role model observational learning tool for stroke recovery and coping (in DVD format).
We have now completed an international multi-site pilot trial, entitled ‘Stroke Self-management Rehabilitation Trial’. This study tested the implementation of a DVD intervention with all study processes tested across recruitment sites in New Zealand, Canada, Singapore, United Kingdom, USA, and India. Secondary aims were to collect process measures about strengths of the intervention, barriers to protocol adherence, participant suggestions for improvements, and preliminary efficacy data.
Findings suggest a self-management approach to stroke rehabilitation delivered via DVD is feasible worldwide with global support from stroke clinicians and survivors of stroke. To better meet the individual needs of each patient, and to maximise uptake, self-management programmes require an individualised approach that can be adapted to meet people’s changing needs.
Information from this pilot trial (and subsequent focus group sessions held in in 2016) is now informing the ongoing refinement of the self-management rehabilitation programme delivered via DVD. Future plans include a full-scale randomised controlled trial and the potential development of an app version of the intervention.
If proven to be effective, this unique observational learning tool may have a vital and positive impact on reducing stroke burden within our communities, as well as worldwide. Findings will be relevant to clinicians, rehabilitation specialists, stroke researchers and policy makers involved in maximizing the recovery of stroke survivors and reducing burden for family caregivers.
Collaborators
- National Institute for Stroke and Applied Neurosciences, AUT, Auckland, NZ – Prof. Valery Feigin, Dr R Krishnamurthi, Dr A Theadom, Associate Professor S Barker-Collo, Dr K Jones
- North Shore Hospital, NZ – Dr Yogini Ratnasabapathy
- University of Otago, Palmerston North, NZ – Dr Anna Ranta
- Griffith Health Institute, Griffith University, Queensland, Australia – Prof. E. Kendall, Dr A. Maujean, Dr C. Ehrlich
- Monash University, Melbourne, Australia – Prof. A. Thrift, A/Prof. D. Cadilhac
- Emory University, Atlanta, USA – Prof. S. Wolf, Assistant Prof. S. Blanton
- School of Physiotherapy, Dalhousie University, Halifax, Nova Scotia, Canada – Prof. M. MacKay-Lyons
- Govind Ballabh (G B) Pant Hospital, New Delhi, India – Prof. M. M. Mehndiratta
- Christian Medical College, Ludhiana, India – Prof. J. Pandian
Funded by NISAN with support from the New Zealand Stroke Education Charitable Trust.
Contact: Kelly Jones
SMART study newsletters
SMART Newsletter December 2013 - Issue #1
SMART Newsletter April 2014 - Issue #2
SMART Newsletter July 2014 - Issue #3
SMART Newsletter November 2014 - Issue #4
SMART Newsletter August 2015 - Issue #5
Fatigue is a common and persistent deficit in up to 92% of stroke survivors that can negatively impact functioning. It is imperative that new strategies be developed to tackle post-stroke fatigue, a debilitating but often overlooked sequelae of stroke. Cognitive and behavioural (educational) interventions for fatigue have been successful in other conditions (e.g. traumatic brain injury, multiple sclerosis, chronic fatigue syndrome), but have not been fully examined in the context of stroke. Building on promising findings from our pilot study, this full-scale randomised controlled trial aims to assess the effect of the intervention on reducing physical, psychological and mental fatigue and improving quality of life in stroke survivors. Family carer quality of life and burden, as well as impact of the intervention on other functional outcomes and costs will also be examined. This trial has potential to improve quality of life and day-to-day functioning for stroke survivors and their families.
Design: Randomised Controlled Trial
Study population
There are opportunities for 200 adults (aged 18 years or older) with clinically significant fatigue at 3 to 18-months after first-ever stroke to take part. A nominated person who helps to take care of the person with stroke can also participate, if available. People with all types of stroke will be included.
Definition
Fatigue is defined as “feeling constantly weary, tired and lacking energy or strength. These feelings and symptoms are present even after a rest or sleep”.
Inclusion criteria
- Clinically significant fatigue at 3 to 18-months after first-ever stroke;
- Living in the study areas (Auckland, Waikato);
- Ability to converse in English;
- Able to provide informed consent.
Investigators
- Kelly Jones (Principal Investigator)
- Valery Feigin
- Rita Krishnamurthi
- Suzanne Barker-Collo
- Irene Zeng
- Braden Te Ao
Timeline: 01 October 2018 to 30 September 2022
Recruitment start date: 01 March 2019
Funded by: Health Research Council of New Zealand (Budget $1.18million)
FASTER key summary of findings
Contact
- For further information, email the study team at faster@aut.ac.nz.
- Associate Professor Kelly Jones Email: kelly.jones@aut.ac.nz; Phone: 021 246 0587.
- Study manager Dr Devaki de Silva Email: devaki.de.silva@aut.ac.nz; Phone: 021 837 175
You can elect to join this international research study, where your data will help us better understand stroke and its risk factors and develop global prevention strategies.
What is RIBURST?
RIBURST is an international collaborative study that aims to better understand the risk factors associated with stroke, heart attack, dementia, and diabetes mellitus and to assess how much influence each risk factor has on the likelihood of having a stroke, heart attack, dementia and diabetes mellitus in the future.
As of 2016, the Stroke Riskometer app already involved over 300 renowned stroke experts from 102 countries, making it the largest international collaborative mobile health project in the world.
You can contribute to this study by submitting your results through the app - this will help researchers better understand stroke, heart attack, dementia and diabetes mellitus to improve the prevention of these devastating disorders within your own and the international community.
The study is conducted according to the internationally accepted Good Clinical Practice Guidelines and relevant regional regulatory (Ethics) Committee requirements. Your participation is completely voluntary. Please see the research section of the Stroke Riskometer app for more information on the study and the consent form.
The study has been approved by Auckland University of Technology Ethics Committee on 22/07/2014 (AUTEC Reference Number 14/201).
Digital technologies sub-study
There is currently a digital technologies sub-study being conducted under the RIBURST umbrella:
This international research programme involves members of the RIBURST consortia who are interested in conducting research using NISAN’s digital technologies. These individual research projects by member countries aim to determine the efficacy and uptake of the PreventS-MD web app for clinicians combined with the Stroke Riskometer mobile app for secondary stroke prevention in adults with TIA or IS.
Investigators
- Professor Valery Feigin (AUT University, Principal Investigator)
- Dr Bala Nair (AUT University, Co-Principal Investigator)
- Professor Bin Jiang (PI from China)
- Dr Jiang Yong (PI from China)
- Professor Li-Ping Liu (Advisor from China)
- Professor Wenzhi Wang (Advisor from China)
- Professor Epifania Collantes (PI from Philippines)
- Professor Rajinder Dhamija (PI from India)
- Professor Mehdi Farhoudi (PI from Iran)
- Professor Şerefnur Öztürk (PI from Turkey)
Contact
- Dr Bala Nair (Co-Principal Investigator and Programme Manager)
Email: bnair@aut.ac.nz, Phone: +64 9 921 9999 ext 6915
RIBURST study newsletters
Stroke and other non-communicable disorders (NCD) such as heart attack, dementia, and diabetes, are major causes of death and disability worldwide. Stroke is up to 90% preventable if the risk factors for stroke are well controlled. PreventS-MD is an electronic patient management system (ePMS) that is built on the Stroke Riskometer™ App - a globally recognised application for assessing risk of stroke. PreventS collects information on stroke risk factors and stroke related outcomes over the previous 12 months, calculates absolute and relative risk of stroke in the next 5 years, and provides patient-tailored recommendations for primary and secondary stroke prevention.
There are 2 parts to this study:
- PRIME – International. Involving global partners on PreventS-MD usability and validation.
- PRIME – NZ. Involving DHBs and GPs and getting the web-app on MedTech and DHB’s systems.
Aim
- to examine clinicians’ as well as patients’ perspectives about the usability of the PreventS app for stroke prevention in clinical practice;
- to update the PreventS system based on their feedback.
Materials and methods
The study involves a survey followed by an interview for the clinicians and an interview only for patients. The survey and interview will take approximately 30 minutes each to complete.
Prospective outcomes
Optimising the PreventS webapp for the needs of clinicians and patients.
Project leader
- Professor Valery Feigin
Project coordinator
- Dr Bala Nair
Research fellow
- Dr Alex Merkin
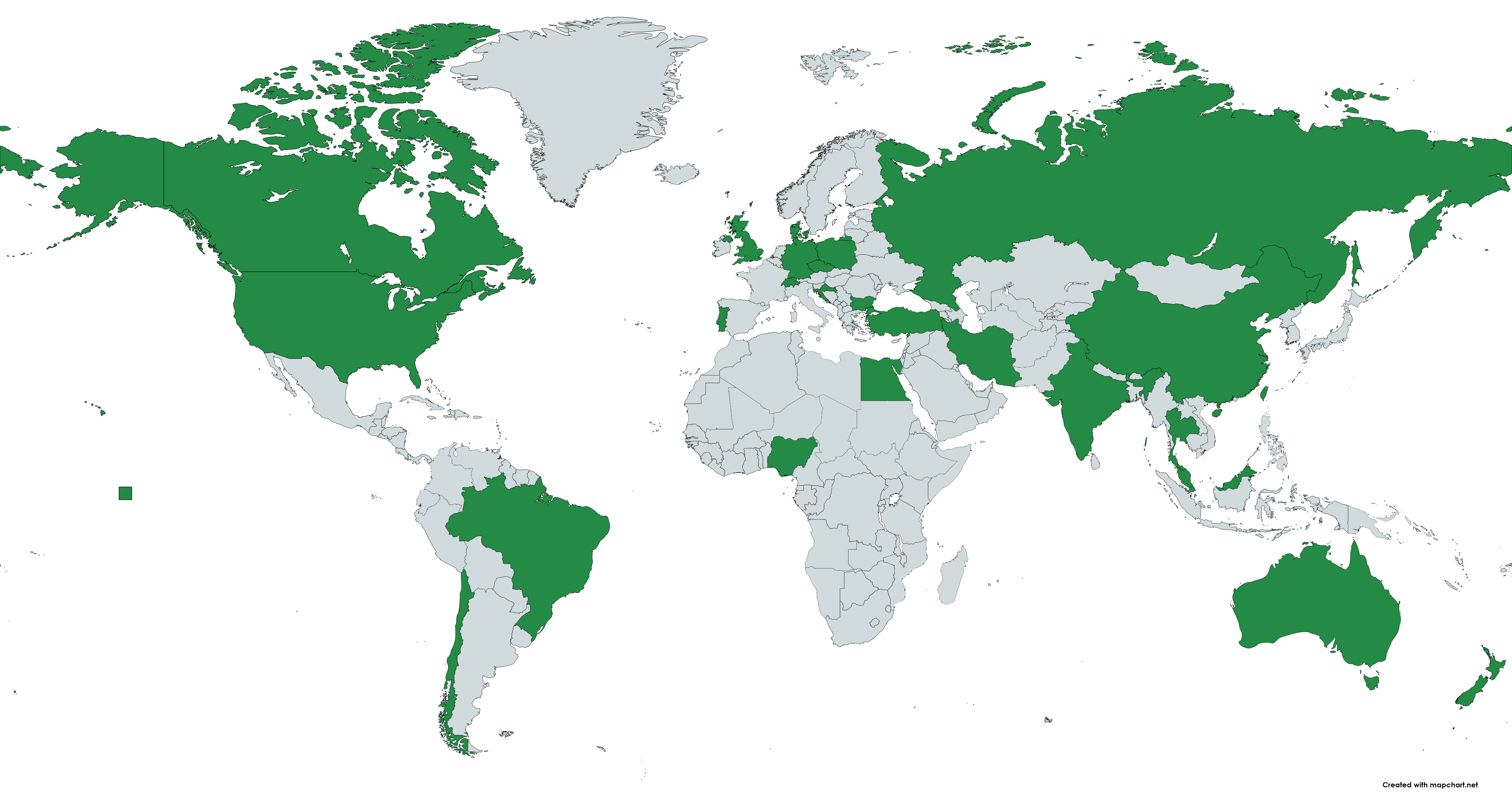
At present, 55 collaborators representing 24 countries (shown in green) have agreed to participate in the PRIME International study, including NZ.